Learn more about retirement home
An introduction to retirement homes is really an introduction to choice. As lifespans extend and lifestyles diversify, older adults and their families want options that balance autonomy, safety, and community. This article pulls together definitions, costs, care standards, and everyday living details so you can compare settings confidently and create a plan that fits your priorities.
What a Retirement Home Is—and Why It Matters
Outline for this guide:
– Overview: definitions, who benefits, types of retirement homes.
– Money matters: costs, contracts, and funding approaches.
– Quality and safety: staffing, care practices, inspections.
– Daily life: amenities, activities, independence, and dignity.
– Choosing well: touring tips, checklists, and transition planning.
A retirement home is a residential community designed for older adults that blends housing, services, and social life in one setting. The term covers a range—from independent living apartments with housekeeping and meals, to assisted living with daily help, to memory care that specializes in dementia support. Some campuses bundle these levels together so residents can move between them without leaving familiar surroundings. That progression matters because needs may change over time, and a plan that anticipates change reduces stress later.
Why is this relevant now? Populations are aging worldwide, and older adults are prioritizing purpose and connection alongside health. Many prefer a home where chores are outsourced, fitness and arts are on the calendar, and transportation is handled. In practical terms, that can mean fewer hospital readmissions due to coordinated care, and more time for meaningful routines. While every community has its own personality, most share core services: meals, housekeeping, maintenance, activities, and some level of care oversight.
Key types often compared include:
– Independent living: private residences plus amenities, ideal for those seeking convenience and social life without daily care.
– Assisted living: personal care (bathing, dressing, medications) layered onto housing and activities.
– Memory care: secure design, structured days, and staff trained in dementia support.
– Continuing care (also called life plan): multiple levels of care on one campus with the ability to transition as needs evolve.
It helps to distinguish a retirement home from a skilled nursing facility. The latter focuses on round-the-clock clinical care and rehabilitation; the former emphasizes residential living with supportive services and variable nursing availability. Neither is inherently “better”—they simply meet different needs. A thoughtful approach starts with current abilities, likely future changes, and preferences about privacy, community size, and location. With those anchors, you can evaluate communities on how well they deliver independence, safety, and meaningful engagement—three pillars that tend to predict satisfaction.
Costs, Contracts, and Financing: Mapping the Money Side
Cost is often the first big question, and for good reason. Monthly rates typically reflect housing, utilities, meals, housekeeping, transportation, and activities; care services are frequently priced separately. In many regions, independent living fees resemble upscale apartment rents with extras attached, while assisted living averages in the mid four-figures per month, with memory care higher due to staffing intensity and safety features. Urban centers and coastal markets tend to command higher rates; smaller towns and rural areas can be more moderate.
What drives price differences?
– Care intensity: hands-on assistance and specialized monitoring add labor costs.
– Apartment type: studio vs. one- or two-bedroom, private vs. shared accommodations.
– Dining model: all-inclusive meal plans vs. flexible points or pay-as-you-go options.
– Amenities: fitness centers, pools, gardens, workshops, and transportation fleets.
– Location: proximity to hospitals, cultural venues, and family.
Contracts vary. Rental agreements resemble standard leases with community rules and service packages. Entrance-fee models involve a one-time payment that may be partially refundable and is paired with lower monthly fees; these are common where multiple care levels are on one campus. Read the details on rate increases, care level changes, deposit policies, and what happens if you need a higher level of care. Look closely at care assessment processes: how added services are triggered, how they’re billed, and how often your plan is reviewed. Transparent communities will show rate sheets, sample invoices, and written policies.
How do people pay? Most combine savings, home sale proceeds, pensions, and retirement income. Some hold long-term care insurance that reimburses specific services once certain eligibility criteria are met. Public programs can support medical or rehabilitative care in particular settings, but they may have limited coverage for assisted living services; rules differ by jurisdiction, so it pays to confirm eligibility early. Practical steps:
– Build a 3–5 year budget with conservative assumptions for annual increases.
– Ask for typical ancillary charges (medication management, incontinence supplies, escort services).
– Compare two or three communities on total cost of care at your likely support level, not just base rent.
– Identify a backup plan if care needs change faster than expected.
Finally, consider value, not just price. A lower base rate that requires many add-ons can exceed the cost of a seemingly higher all-inclusive model. If transportation replaces a car, if on-site clinics reduce off-site appointments, and if meals and utilities consolidate multiple bills, the total household budget may even out. Aim for clarity, not assumptions, and put everything in writing before you sign.
Care, Safety, and Quality: What to Look For Behind the Brochure
Quality is visible in details: how staff greet residents by name, how quickly call buttons are answered, how dining rooms sound during mealtimes. It is also built on procedures you cannot always see. Ask about staff training, supervision, and turnover. In assisted living and memory care, look for education in dementia techniques, medication administration, fall prevention, and infection control. Background checks, continuing education, and mentorship programs indicate a community that invests in stable, skilled teams.
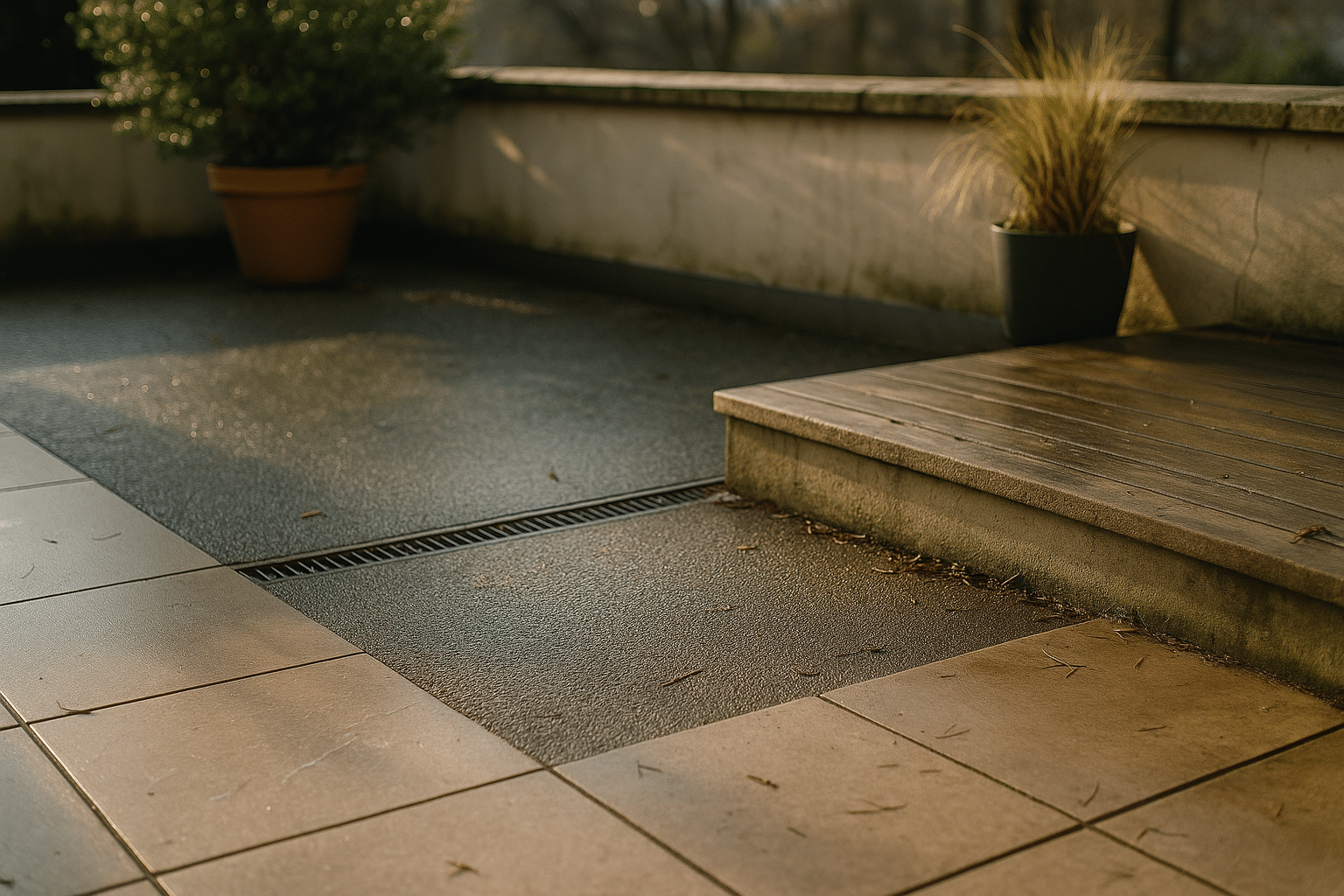
Safety starts with design: grab bars, non-slip flooring, clear wayfinding, good lighting, and secure outdoor spaces. In memory care, layouts that reduce confusion, controlled entries, and calming sensory cues matter. Technology can help—pendant alerts, motion sensors, and electronic record keeping—yet human oversight remains central. Dining safety is part of the equation: hydration cues, appropriately textured foods, and attentive monitoring during meals support health and reduce aspiration risk.
Quality indicators to request:
– Recent inspection or licensing reports and how issues were resolved.
– Staffing patterns by shift, including licensed nurses where applicable.
– Response time benchmarks for call systems and care alerts.
– Incident tracking: falls, medication errors, and how trends are addressed.
– Resident and family satisfaction survey summaries and action plans.
Ask about care coordination with outside physicians, therapy providers, and hospitals. A strong handoff plan—complete medication lists, timely communication, and follow-up after hospitalizations—can reduce complications. Equally important: how often care plans are updated and who participates. Residents should be central in decisions, with family involved as desired. In memory care, observe how staff redirect instead of restrain, how they use life-story information to tailor routines, and how they honor dignity during personal care.
Emergency readiness deserves attention. Request policies for severe weather, power outages, and public health events. Supplies, backup generators, and clear communication trees can make a critical difference. Finally, trust your senses: consistent cleanliness without harsh odors, respectful language, relaxed body language, and residents engaged in authentic activities are everyday signals of a well-run home.
Lifestyle, Community, and Well-Being: Beyond the Floor Plan
The heart of a retirement home is how it feels to live there. Lifestyle programming turns a building into a community by offering choices that reflect different personalities. Some residents thrive with art studios, travel clubs, and gardening plots; others prefer quiet reading rooms, scenic walks, and small conversation circles. Good calendars balance variety with routine, offering fitness classes, lectures, intergenerational projects, and volunteer opportunities. Transportation links these activities to the broader neighborhood, reducing reliance on a personal car and expanding social life.
Amenities matter, but usefulness matters more. A modest gym that is accessible and staffed can be more valuable than a grand space that sits empty. Dining flexibility—multiple venues, adjustable meal times, and options for special diets—keeps mealtime enjoyable. Outdoor access is underrated: patios, walking paths, and shaded benches invite movement and vitamin D. In memory care, sensory gardens and familiar household layouts can ease anxiety and encourage safe exploration.
Social connection is a health factor in its own right. Research has associated loneliness with increased risks to physical and cognitive health, which is why intentional community-building is not just nice-to-have. Look for:
– Resident-led clubs, where people shape activities rather than just attend.
– Opportunities to contribute skills, from mentoring to music to crafts.
– Spaces designed for small groups, not only large events.
– Support for spiritual life and quiet reflection as desired.
Personalization makes a new place feel like home. Ask how residents can decorate their spaces, bring pets, or continue cherished routines. Technology support—help with video calls, streaming, or smart-home devices—keeps people connected to family and interests. Privacy should be respected; doors should close, schedules should be negotiated, and staff should knock. When independence is honored, people often participate more freely, which supports mobility, appetite, and mood. In this way, lifestyle features and well-being reinforce each other, day by day.
Choosing Confidently: Tours, Checklists, Red Flags, and Your First 90 Days
The selection process is clearer with a plan. Start by listing must-haves, nice-to-haves, and non-negotiables. Add a realistic budget with room for care increases. Narrow your list by location and size—some prefer intimate settings, others enjoy larger campuses. Schedule tours at different times of day to see peak activity and quieter moments. Bring a notebook and compare the same factors at each visit to avoid being swayed by staging or a single conversation.
Questions to ask on every tour:
– What is included in the monthly rate, and what is billed separately?
– How are care needs assessed and re-evaluated?
– What is the average response time to calls for assistance?
– How does the community handle night staffing and emergencies?
– Can we see sample menus, activity calendars, and a recent inspection report?
Common red flags include vague answers, inconsistent cleanliness, residents who appear disengaged during multiple visits, and abrupt staff turnover without explanation. Conversely, green flags include candid discussions about challenges, visible teamwork, and residents who greet staff comfortably. Ask to speak with a couple of residents or family council members, if available, and request a copy of community rules and a plain-language summary of the contract before committing.
Planning the move helps it feel like a fresh start rather than an upheaval. Create a floor plan to scale and choose furnishings that fit pathways and safety needs. Pack “first-night” essentials separately: medications, important documents, glasses, hearing aids, chargers, toiletries, and a few favorite photos. Notify healthcare providers, update addresses, and set up mail forwarding. Arrange medication reconciliation with the new care team so orders and dosages are precise from day one. During the first 90 days, schedule check-ins with staff to adjust the care plan, try multiple activities, and meet neighbors. Small rituals—morning coffee in the courtyard, a weekly bridge game, a call with family after dinner—help a new routine take root.
Conclusion for older adults and families: Choosing a retirement home is not a single decision but a series of thoughtful steps. Define your priorities, verify quality, and look for a community that protects independence while offering the right safety net. When the environment, services, and budget align, everyday life becomes easier and more satisfying. With a clear checklist and patient comparisons, you can move from uncertainty to a confident, comfortable next chapter.